Trauma, illness, mental health care – and space concerns – all forces in Pen Bay’s ED overhaul
 A rendering of the new entrance for the Pen Bay Medical Center emergency department. The project begins July 5.
A rendering of the new entrance for the Pen Bay Medical Center emergency department. The project begins July 5.
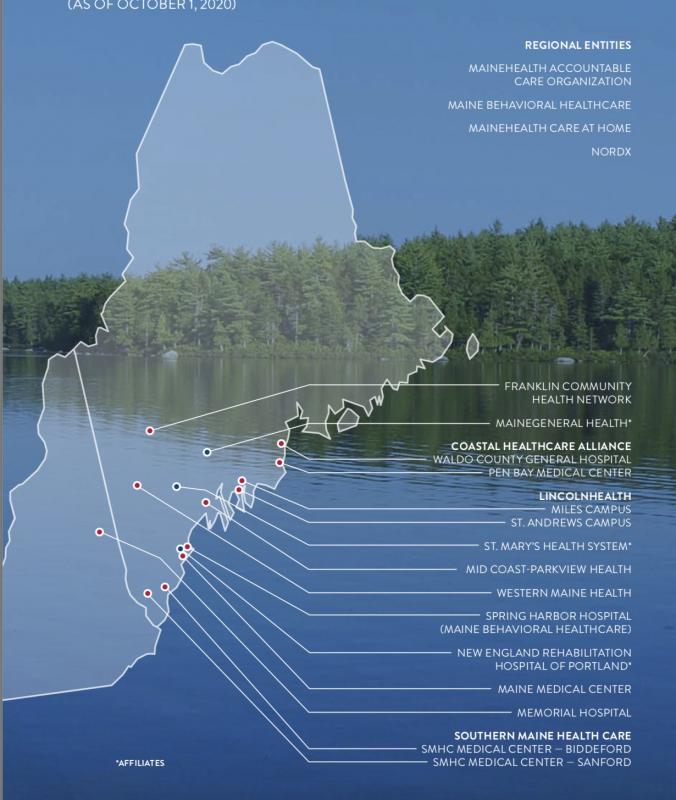 Pen Bay Medical Center is part of MaineHealth, based in Portland. The umbrella nonprofit oversees a statewide network of small nonprofits, including Pen Bay, and the nearby hospitals of Miles, in Damariscotta, and Waldo County General, in Belfast. According to MaineHealth’s 2020 annual report, MaineHealth is the largest health system in northern New England and provides preventive care, diagnosis and treatment to 1.1 million residents in Maine and New Hampshire.
Pen Bay Medical Center is part of MaineHealth, based in Portland. The umbrella nonprofit oversees a statewide network of small nonprofits, including Pen Bay, and the nearby hospitals of Miles, in Damariscotta, and Waldo County General, in Belfast. According to MaineHealth’s 2020 annual report, MaineHealth is the largest health system in northern New England and provides preventive care, diagnosis and treatment to 1.1 million residents in Maine and New Hampshire.
 A rendering of the new entrance for the Pen Bay Medical Center emergency department. The project begins July 5.
A rendering of the new entrance for the Pen Bay Medical Center emergency department. The project begins July 5.
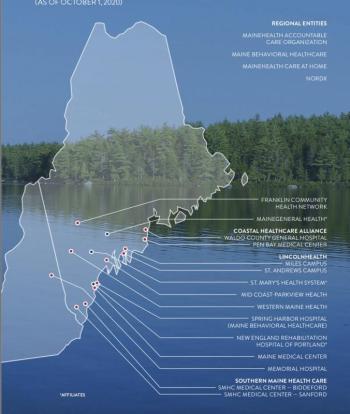 Pen Bay Medical Center is part of MaineHealth, based in Portland. The umbrella nonprofit oversees a statewide network of small nonprofits, including Pen Bay, and the nearby hospitals of Miles, in Damariscotta, and Waldo County General, in Belfast. According to MaineHealth’s 2020 annual report, MaineHealth is the largest health system in northern New England and provides preventive care, diagnosis and treatment to 1.1 million residents in Maine and New Hampshire.
Pen Bay Medical Center is part of MaineHealth, based in Portland. The umbrella nonprofit oversees a statewide network of small nonprofits, including Pen Bay, and the nearby hospitals of Miles, in Damariscotta, and Waldo County General, in Belfast. According to MaineHealth’s 2020 annual report, MaineHealth is the largest health system in northern New England and provides preventive care, diagnosis and treatment to 1.1 million residents in Maine and New Hampshire.
ROCKPORT — An overhaul and expansion of the Pen Bay Medical Center’s Emergency Department is due to get underway July 5, a redesign that the hospital said will incorporate a more secure and efficient response to medical trauma, illness and mental health crises.
The latter has emerged as a national healthcare concern, and one intensified by COVID 19.
Health care and social service organizations are directing money into programs and facilities to tackle myriad mental and behavioral health challenges and Pen Bay’s ED improvements are one piece of a response to a systemic problem that is only getting larger, said Mark Fourre, president Pen Bay Medical Center/Waldo County General Hospital, and former emergency room physician himself.
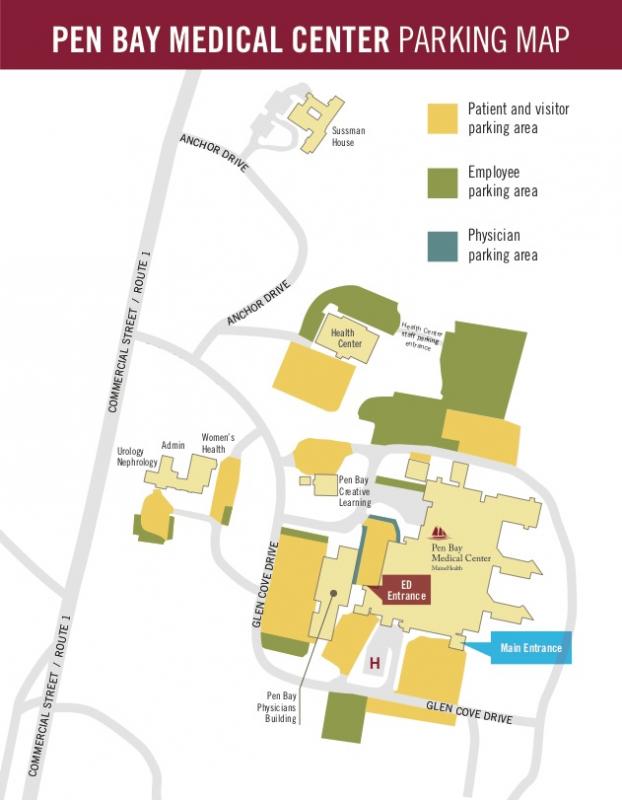
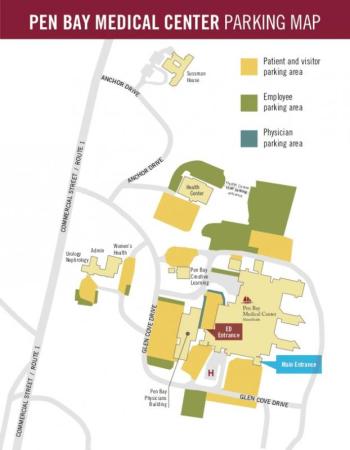
The Pen Bay ED, which is a core element of the Rockport medical campus, will not pause functioning as the area’s emergency care facility during its rebuild, but there will be new temporary entrances and parking as the two-year, $9 million project takes shape (see sidebar).
Built in the mid-1970s, the 99-bed PBMC has expanded on its 63-acre parcel, which lies between Route 1 and the ocean.
Last year, a new $16 million physicians’ office building was built on the Rockport campus. Eight years ago, Pen Bay opened the then newly constructed 9,740-square-foot hospice facility, the Sussman House.
The existing ED, however, has remained primarily unaltered since 1997. Minor adjustments were made here and there, with hallways and doors relocated and new rooms carved into the existing footprint; yet, all have been fixes, not changes.
“It is way too small,” said Fourre “We are still able to deliver high quality care. But it is a struggle to do so, and the patient experience on a busy day is not something we feel is appropriate or up to our expectations, or the patient’s expectations.”
With 13 exam rooms, the ED currently handles approximately 22,000 patients a year; 55 is the daily average, although that increases to 70 during the summer season.
Patients stream in from the broader Midcoast — the peninsula communities of Cushing, Friendship and Port Clyde, the islands of Penobscot Bay, inland towns of Washington, Warren and Union, as well as the more populated service centers of Rockland and Camden.
Who shows up in the ED reflects the region’s way of life and its economies. Lobstermen, loggers and carpenters rush in with occupational wounds. The elderly who live alone, or in nursing homes, are transported daily to the ED. They may have fallen and been found the next day on the floor, or they suffered a stroke.
Vehicular crashes are regular occurrences on local highways and rural roads. Hikers, bicyclists and skiers filter in from the outdoors with injuries. Assault and domestic violence victims, and drug overdose patients, are not unusual to treat.
There are also the incarcerated who need medical help, inmates from the maximum security Maine State Prison in Warren, or the Knox County Jail in Rockland.
Then there are the visits of those troubled by nagging coughs and pains. Maybe the flu turned into pneumonia, or the dysentery acquired on trip to the tropics just won’t go away.
Add to the mix a growing number of patients suffering mental health crises, and who seek help at the hospital’s Psychiatric and Addiction Recovery Center (PARC).
The ED sees it all, 24/7.
And at the busiest times, which can spontaneously erupt, patients line hallways on gurneys, with no privacy, as medical staff and other patients pass by. And it is hard to adequately monitor patients in the hallways, said Fourre.
“Daily census and activity logs demonstrate periods of time where there have been 22 patients in the ED with 13 rooms,” wrote Will Gartley, of Gartley and Dorsky Engineers, the Rockport company that represented MaineHealth at municipal planning board meetings earlier this spring.
“We’ve known for some time we’ve needed more emergency rooms,” Fourre said. “Plus, the doctor and nursing area is congested.”
The latter is a small square space in the middle of the ED. There, staff lean over computers, doing paperwork or watching cameras that keep an eye on patients in various rooms. They peer through the glass windows to watch patients in the hallways, confer with colleagues and first responders who wheel patients in from ambulances, or law enforcement personnel accompanying prisoners.
Fourre looks forward to the redesign, which is under the direction of E4H Architects, healthcare and health science and technology architects whose primary office is in Boston, but have offices in New York City, Texas, North Carolina, Vermont as well as Portland.
The Rockport Planning Board approved the expansion project in May, and the building permit was due to be issued in late June. Lead contractor is the Lewiston-based Hebert Construction.
Hebert recently completed the 41,513-square-foot Health Center at Pen Bay’s Rockport campus. and the Watson Medical Arts Building, in Damariscotta, and also part of MaineHealth. That 3-story steel frame structure is approximately 39,500 square feet in size.
Pen Bay ED upgrades involve expanding the emergency room footprint by 5,600 square feet, making the ED a total of 8,000 square feet in size.
“Volume trending data indicate the need for expansion as well as specific attention to a dedicated behavioral health component,” said Pen Bay, in its submissions to the Rockport Planning Board.
Demographic trends shape the changes
Hospital emergency departments have changed dramatically over the decades, but the public’s lexicon dates back a century.
“Going to the ER is what people say,” said Fourre. “And that stands for emergency room. That’s because when emergency services began, it was a room. You were either able to drive, or walk, to it. They called the only laying-flat vehicle in town, which was at the funeral home – they were the ambulance service.”
These days, a substantial part of an ED’s function is to care for trauma patients.
But, there are other indicators of changing demographic and social trends.
“People are bigger and care is more complex,” said Fourre. The population is, he said, “unequivocally older.”
That requires more complicated levels of care, more people in the room tending to the patients, and more pieces of advanced technological equipment.
“Patients are increasingly sicker,” added Fourre — high blood pressure, diabetes, pulmonary disease — they have become common ailments that can spin out of control.
Even on the hospital floors, reasons for admittance have changed. Where once ward beds would have been occupied by post-surgery patients, those indviduals are now recovering at home, a consequence of more out-patient day surgeries.
But in those beds are older patients.
“People’s nervous systems are what are now giving out,” said Fourre. ‘They are now living to develop dementia, which is complex to care for.”
Along came a pandemic
Then came COVID-19, and with it, a “behavioral health epidemic of remarkable size,” said Fourre. “Initially, people called it a shadow pandemic but it is more than that now. We have adults and children waiting in an emergency departments for placement in a psychiatric facility. That has really exacerbated emergency departments across the country and locally. Especially at Pen Bay. We are very fortunate to have the PARC, which is a combined substance abuse disorder and psychiatric patient facility; however, that tends to be a little bit of draw because people know they can get good care here.”
Adults and children of all ages, and across all spectrums, were affected.
“There are immediate behavioral health impacts from this pandemic, as well as potential long-term effects as people grapple with disruption, isolation, traumatic experiences, grief, and economic instability,” said Dr. Jessica Pollard, Director of the Maine Dept. of Health and Human Services, more than a year ago.
On June 23 of this year, the Maine Attorney General’s office released drug overdose data reporting a 33 percent increase of deaths caused by drugs from 2019 to 2020. The report attributed 504 Maine deaths to drug overdose in 2020, compared to 380 in 2019. Fentanyl is the predominant drug associated with the overdoses.
Currently, Pen Bay’s ED often cares for patients waiting for placement in other mental health care facilities, and with behavioral crises, a patient is isolated in a regular exam room, with a hospital security guard at hand.
“There are patients, when the PARC is full, or the patient isn’t appropriate for that particular hospital, for instance, no children are admitted to Pen Bay, then it becomes a long process of trying to get them admitted to an appropriate behavioral health unit,” said Fourre.”
That leaves less room for other patients, resulting in crowded hallways.
Ideally, said Fourre, a patient suffering mental/emotional distress, “would be able to ride into an emergency department, be promptly placed into the appropriate care setting, have a nurse do an initial triage, begin some intervention as identified by the nurse, be seen by an emergency provider promptly, and have the diagnostic plan outlined and get to a decision about whether they are going home or coming into the hospital, and initiate treatment as appropriate.”
And, he added, “you’d like to be able to do that in a space both comfortable and efficient.”
The improvements
Post-redesign, the new ED is to provide three rooms for patients undergoing crisis behavioral challenges. Those rooms, said Fourre, will be in an area that is contained, and able to be locked. They are not, he said, designed predominantly for a person for medical emergencies, such as heart attacks or abdominal pain.
The goal, he said, is to establish an ED that is comfortable and safe, and which has an improved flow of services – room to maneuver, medical supplies at close hand, and a clear line of sight into rooms. There will be more cameras positioned throughout the facility, with spaces designated for more specific purposes — “a lot of efficiencies built in,” said Fourre.
That includes 15 more sinks, two showers and a drinking fountain, according to Maine Water, the company that provides water to Pen Bay.
“Based on the criteria that has been presented, MWC does have sufficient capacity in the area from the existing 16-inch ductile iron public main on Commercial Street to serve the needs of this project,” said Maine Water, in its report to the town about the ED expansion. “Additional infrastructure improvements may be required at the expense of the developer to meet the overall needs of this project.”
“The new ED is greeted with enthusiasm by everybody,” Fourre said. “The care team does have to to get used to it, and may end up walking more than they are used to, just because it’s bigger and designed to improve flow.”
He said the pre-design work included gathering insight from those working in the Pen Bay ED. A committee had been formed comprising doctors, nurses, assistants, and maintenance staff, he said.
MaineHealth’s mission, the large nonprofit says, is, “dedicated to improving the health of our patients and communities by providing high-quality affordable care, educating tomorrow's caregivers, and researching better ways to provide care.”
Expanding on that, Fourre said he works to instill the passion for service through the two medical campuses he oversees.
“Throughout my career, which involves becoming an emergency physician, training emergency physicians as a residency director, being an ED director, being a chief medical officer, and now the president of a hospital, that whole concept of service is central to everything,” he said.
“When I recruited medical students for residency and when I recruited emergency physicians, and now when I recruit any type of physician, that’s what I’m looking for — is somebody who has that clear focus in terms of what their mission is. The mission for MaineHealth is working together so our communities are the healthiest in America, and the ED is there to support that mission.”
Reach Editorial Director Lynda Clancy at lyndaclancy@penbaypilot.com; 207-706-6657
Event Date
Address
United States