MaineHealth hospitals slammed with COVID-19 cases, appeal to public to vaccinate, get boosters
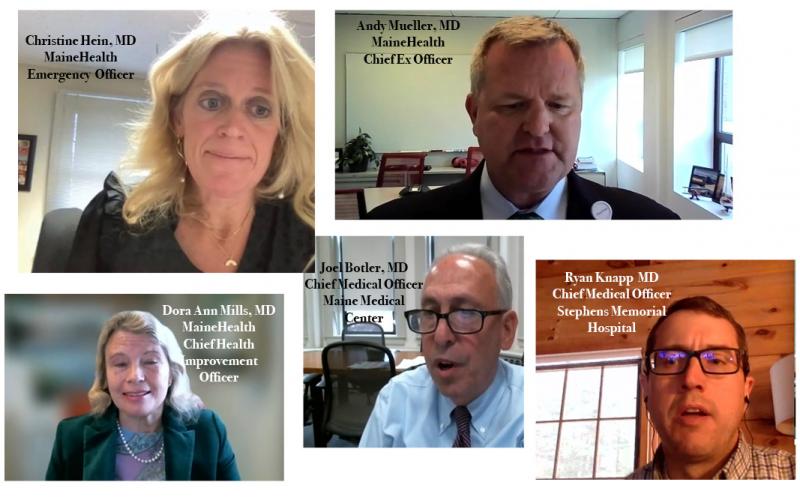
MaineHealth invited Maine media to a Wednesday morning Zoom news conference to describe a strained statewide hospital system that is struggling to figure out how care for more ill patients.
“We’re running out of straws,” said Andrew Mueller, MD, MaineHealth Chief Executive Officer. “There are not a lot of options left.”
Since Thanksgiving, there has been a steadily upward trend in the number of COVID cases, the brunt of which will not likely be seen for another several weeks, the MaineHealth executive staff agreed, speaking at the news conference.
“As much as we hoped we were wrong, this appears to be a fairly steady trend as a result of the Thanksgiving holiday,” said Mueller. “So we don’t think we’ve seen the full breadth of this surge and probably won’t for another two to three weeks, and then of course we fear that will lead into what will ultimately become a post-Christmas and New Year’s surge.”
He said: “This really largely is a pandemic for the unvaccinated.”
Currently, 90 percent of those in the critical care units are unvaccinated, said Mueller. The vaccinated have less risk for severe illness, requiring hospitalization.
The pandemic, now two years plaguing the world, plus a labor shortage of healthcare workers, has resulted in a storm of limited care capacity. Hospital intensive care units are overrun with sick patients and nurses, doctors and staff are exhausted. Some are quitting, others are getting infected with COVID.
Add to that an emerging crisis in behavioral health, with patients suffering emotional and mental illnesses also filling hospitals. That is its own pandemic, said Mueller.
“We need everyone to get vaccinated,” he said, again and again through the hour-long press conference. “We really need the help.”
Pen Bay Medical Center, in Rockport; Waldo County General Hospital, in Belfast; and Miles Memorial Hospital, in Damariscotta, are not immune. Being under of the MaineHealth nonprofit medical care system, the three Midcoast hospitals work with others around the state to supply beds, or turn to others when they are at capacity.
The sickest COVID-19 patients that previously would have been transported to Maine Medical Center in Portland for acute care are staying put. There is no room left at Maine Med.
“Smaller hospitals are now taking more of the acute care,” said Ryan Knapp, chief medical officer at Stephens Memorial Hospital, in Norway.
It is a matter of finding beds anywhere, even across the state line in New Hampshire. Stephens, a 25-bed hospital, has been, “running over capacity over the last two weeks,” said Knapp.
“In the beginning of the pandemic, many COVID cases were in urban areas,” he said. “Now a significant burden is in rural counties, where there are very low vaccination rates.”
Reported Dec. 8, there are 367 hospitalized in Maine with COVID-19. Of them, 110 are in critical care and 59 are on a ventilator.
MaineHealth had 116 patients in hospitals across its system being treated for COVID-19, 82 of whom where unvaccinated. The proportion of unvaccinated patients in an intensive care unit was higher, with 39 out of 48 not having been immunized, said MaineHealth. Of the 20 patients on a ventilator, all but three were unvaccinated.
NorDx, the Scarborough lab for MaineHealth, is processing 4,000 to 5,000 COVID tests a day, said MaineHealth Chief Health Improvement Officer Dora Ann Mills. A year ago, at the pandemic’s height, the lab was processing 3,000 day.
And, there are fewer health care workers. Currently, there are 30,000 traveling nurse positions that remain open.
“There is a huge workforce problem across the country,” said Mueller.
On Monday, Dec. 6, Maine Med was at full capacity, and diverting patients to other facilities.
“We are doing everything possible to increase capacity,” said Joel Botler, MD, chief medical officer at Maine Medical Center. The hospital is now converting six surgical rooms to ICU rooms. That’s in addition to the six that had already been repurposed.
On Dec. 6, the hospital was caring for 50 patients with COVID-19, and 10 under investigation for the virus. Six were in the ICU; 13 were critically ill but not in ICU. Fifteen were on ventilators.
“On average in the past, we may have had three on ventilators,” said Botler.
The pandemic and healthcare workforce shortage has resulted in elective surgeries — hip and joint replacements — anything that requires a patient to spend a night in the hospital post-surgery, being postponed.
Currently, 50 percent of MaineHealth elective surgeries have been postponed. That’s 25 fewer surgeries per day, said Botler.
“The backlog is closer to 2,000,” said Mueller.
Although those surgeries are labeled nonemergent, or elective, meaning they do not constitute a medical emergency response, they are not insignificant.
“These are all patients in a lot of pain,” said Mueller.
Christine Hein, an emergency room doctor at Maine Medical Center, said the situation is unprecedented.
“Most of our emergency department beds are taken up,” she said. “We don’t have the ability to provide the same level of care in our waiting rooms and hallways.”
She said health care has been managing the pandemic for two years but, “it is coming to the point we all fear we are going to be making difficult choices,” she said.
The hospitals are, “working creatively to improve this, but best thing we can do is get people vaccinated,” Hein said.
Mills said Maine, with the help of public nurses, has been administering vaccines to students in schools. So far, 9,000 doses have been administered in schools, mostly elementary school students during the school day.
Any contingency plans for an offsite temporary hospital are no longer on the front burner.
“That is the crux of the problem,” said Mueller. “The challenge is not finding the space but finding qualified healthcare workers.”
Even calling in the National Guard, as Gov. Janet Mills announced she was doing today, does not resolve the issue, he said.
Mills announced mid-afternoon that she was activating 75 additional National Guard members to serve in non-clinical support roles. They are to support: “nursing facilities and swing bed units that accept patients discharged from hospitals experiencing critical care capacity challenges. Enhancing the ability of these ‘decompression sites’ to accept more patients will allow hospitals to safely discharge more individuals, relieving a bottleneck that will then allow hospitals to provide inpatient care for more people with COVID-19 and ensure delivery of health care for other serious health problems.”
They are also to help administer monoclonal antibody treatments to help, “keep Maine people out of critical care, preserving intensive care unit (ICU) capacity.”
Mueller emphasized that the labor shortage and the virus’ persistence in the population is the problem, urging again, “We need everyone to get vaccinated.”
“More people are showing up seeking care, and that’s going to continue for a long time,” said Mueller.
There are many more patient in their 50s in the ICU, said Hein, and the, “severity of illness is the greatest we have seen since the onset of the pandemic.”
The sickest patients she has recently seen are those in their 20s and 30s.
Other hospitals, including the Mid Coast Hospital in Brunswick, are caring for a similar demographic. There, six patients are on ventilators, “which is a high number for us, in an 11-bed ICU,” said Christopher Bowe, chief medical officer.
That hospital has had a large number of patients in their 40s, and they are often, “proning,” turning people onto their stomachs, to breath more easily.
The older population has the highest vaccination rate, and “we are seeing them less,” he said.
At the Rockport, Belfast and in Damariscotta hospitals, the connection with the rest of the MaineHealth hospitals is strong.
“From our shared conversations on a daily basis, the volumes fluctuate in all of those facilities with the rest of us, so there are certain days that Pen Bay has been able to have some capacity for intake conditions from Maine Med, or Midcoast here in Brunswick, or our colleagues at Stephens,” said Bowe. “Then there are other days when their capacity is stretched thin and they need to send patients to us, and that availability for the next available inpatient bed for the patient who needs it has really floated throughout the system, each day which region has a few beds available.”
When taking care of COVID patients, Hein said, “We spend a lot of time talking about mortality and then morbidity,” the lingering illnesses of a COVID infection.
“The emotional toll is significant for the staff, when you are faced with delivering the news when someone has severe advanced COVID,” she said.
“OK, what is the plan,” they are asked. “The plan was you hopefully could of gotten a vaccine and could have prevented severe disease,” said Hein.
Every day, health care workers are putting their own health at risk, said Botler.
“They are tired and work so hard, and continually hang in there despite long hours....,” he said. “I can’t tell you how big their hearts are.”
Increasingly, they are also facing physical violence, just to do their jobs, he said.
“Part of our message today is to really implore our community, in a heartfelt way: Kindness matters,” said Mueller. “These are great heroes who are doing so much for all of us. Please do your part to be kind to them and respect them.”
Reach Editorial Director Lynda Clancy at lyndaclancy@penbaypilot.com; 207-706-6657